Comprehensive Revenue Cycle Management
Optimize your healthcare revenue cycle with our end-to-end RCM solutions and expert services.
Our RCM Services
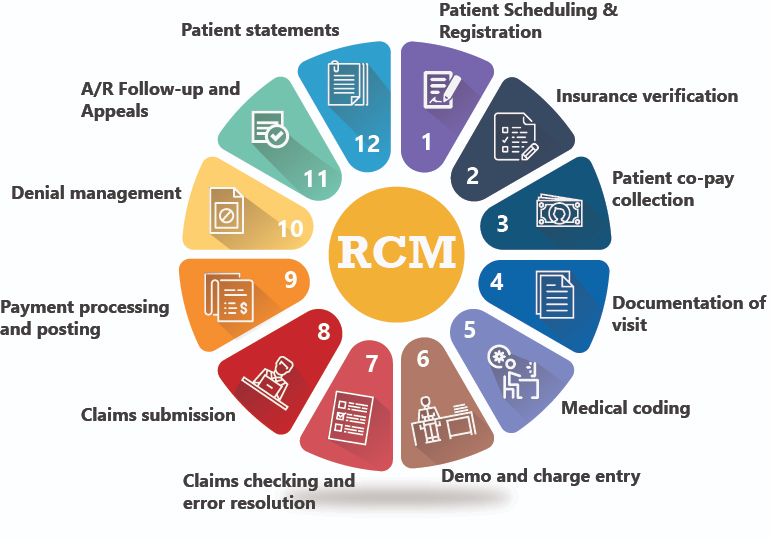
Our comprehensive Revenue Cycle Management (RCM) services provide healthcare providers with a seamless solution to manage every stage of the patient care journey—from initial registration and appointment scheduling to billing, claims processing, and final payment collection. By leveraging tailored automation solutions, we streamline each phase of the revenue cycle, minimizing manual inefficiencies, reducing administrative errors, and enhancing operational workflows.
Through our detailed, targeted reports, we offer deep insights into the financial health of your practice, helping you gain a clear understanding of its current status and growth trajectory. With the combined power of automation, AI, and advanced software tools, we ensure your practice operates with maximum efficiency and effectiveness, delivering consistent, reliable support throughout your revenue cycle.
Patient Access & Registration
Patient Verification
- Seamless patient information verification
- Detailed insurance policy analysis
- Coverage limits & co-pay insights
- Network status confirmation
- Accelerated claim approvals
- Reduced billing discrepancies
Authorization Management
Simplifies obtaining prior authorizations for medical procedures, ensuring all necessary documentation is submitted promptly.
- Reduces delays in treatment
- Minimizes administrative burdens
- Tracks authorization status
- Provides timely updates
- Prevents claim denials
- Enhances cash flow
Charge Capture & Charge Entry
Coding Management
Our team ensures the meticulous management of coding processes to prevent revenue loss and missed income opportunities.
- Automated CPT/ICD code validation
- Compliance with latest guidelines
- Accurate patient demographics
- Secure EDI claim transmission
- Reduced human error
- Streamlined coding workflow
AI-Driven Coding Suggestions
Beyond basic coding, our automated system provides up-coding and add-on coding suggestions based on detailed office notes and the patient’s treatment.
- AI-driven insights for accurate coding
- Maximizes revenue potential
- Reflects complexity of care provided
- Automated code suggestions
- Detailed office notes analysis
- Patient treatment-based recommendations
Claims Management
Insurance Guideline Tracking
Our system continuously tracks changes in insurance guidelines, AAPC, and CMS publications. Automation ensures updates are promptly identified and our team is automatically alerted when new guidelines affect billing or practice protocols.
- Automated compliance updates
- Proactive alert system
- Maximizes reimbursement opportunities
- Reduces manual effort
- Keeps practice compliant
- Timely guideline implementation
Accounts Receivable (A/R) Management
Accounts Receivable (A/R) Management
Our Accounts Receivable (A/R) Management solutions are designed not just to manage outstanding balances, but to transform your revenue cycle through smart automation, AI-driven insights, and strategic interventions.
- AI-driven claim resolution
- Revenue recovery optimization
- Denial prevention strategies
- Automated follow-up systems
- Real-time A/R analytics
- Strategic payment interventions
Rejection Management
We deploy automated claim scrubbing tools that pre-validate data for common errors before submission, dramatically reducing front-end rejections.
- Real-time rejection dashboards
- Machine learning pattern detection
- Automated claim scrubbing
- Clearinghouse optimization
- Payer connection management
- Cash flow protection
Denial Management
Using predictive analytics, we anticipate denial trends and automate triaging based on denial reason codes, payer behavior, and claim value. Intelligent routing ensures that high-value or time-sensitive denials are prioritized.
- Predictive denial analytics
- Intelligent claim triaging
- Payer behavior analysis
- Network participation verification
- Authorization tracking
- Documentation gap detection
Payment Posting
Automated Payment Processing
With automation, both payment posting and reporting become more accurate, timely, and scalable. This eliminates manual errors, accelerates reconciliation, and ensures consistency across systems. Ultimately, it strengthens financial visibility, enhances decision-making, and supports long-term revenue growth.
- Error-free payment processing
- Real-time data synchronization
- Scalable reporting solutions
- Enhanced financial visibility
- Accelerated reconciliation
- Data-driven decision support
Payment Insights
A well-managed payment posting process provides real-time insights into revenue performance and enables quicker decision-making for follow-ups or appeals. It also ensures that patient accounts reflect the correct remaining balances, making secondary billing and patient collections more transparent and efficient.
- Real-time revenue performance analysis
- Faster decision-making for follow-ups
- Accurate patient balance tracking
- Transparent secondary billing
- Efficient patient collections
- Payer behavior trend analysis
Key Features
Comprehensive solutions to optimize your revenue cycle
Eligibility Verification
Real-time insurance eligibility checks and benefit verification.
Claims Management
End-to-end claims processing and tracking system.
Payment Posting
Automated payment posting and reconciliation.
Denial Management
Proactive denial prevention and appeals handling.
Our Approach
Strategic methodology for optimizing revenue cycle performance
Process Automation
Automated workflows for increased efficiency and reduced errors.
Expert Team
Dedicated RCM specialists with deep industry knowledge.
Performance Analytics
Comprehensive reporting and analytics for continuous improvement.
Why Choose Our RCM Services?
Experience excellence in revenue cycle management with our comprehensive solutions
Faster Payments
Accelerated cash flow through optimized billing processes and reduced AR days.
Increased Revenue
Maximize reimbursement through improved claims accuracy and denial prevention.
Compliance Assured
Stay compliant with healthcare regulations and payer requirements.
Data Analytics
Actionable insights through advanced reporting and analytics capabilities.